Lumbar Fusion Rehab Protocol⁚ A Comprehensive Guide
This guide details a structured rehabilitation program for lumbar fusion surgery patients. It outlines four phases encompassing wound care, pain management, mobility progression, strengthening, and return to functional activities. Each phase includes specific goals, exercises, and precautions to ensure optimal recovery and minimize complications. The protocol emphasizes a gradual increase in activity levels and incorporates posture education for long-term success. Consult your healthcare provider for personalized guidance.
Phase 1⁚ Immediate Post-Operative (0-4 Weeks)
Wound Healing and Protection⁚ The initial focus is on protecting the surgical site and promoting wound healing. This involves meticulous incision care, following prescribed dressing changes, and avoiding any activities that could strain the incision. Pain management is crucial during this phase, utilizing prescribed medications and potentially employing modalities such as ice or heat therapy as directed by your healthcare provider. Early mobilization is encouraged, but movements must be gentle and within pain tolerance to prevent excessive stress on the surgical area. Deep breathing exercises and coughing techniques are taught to prevent pulmonary complications, common after surgery.
Pain Control and Mobility Progression⁚ Pain control is paramount; medication adherence is essential. Gentle range-of-motion exercises begin, focusing on maintaining joint mobility while avoiding any forceful movements. Patients are educated on proper body mechanics, such as bending at the knees and avoiding twisting. Simple, pain-free exercises such as ankle pumps and heel slides are introduced to promote circulation and prevent stiffness. Transfer training (moving from bed to chair, etc.) is initiated with assistance as needed, emphasizing proper body positioning to protect the spine. The goal is to gradually increase mobility while carefully monitoring pain levels and preventing complications.
Wound Healing and Protection
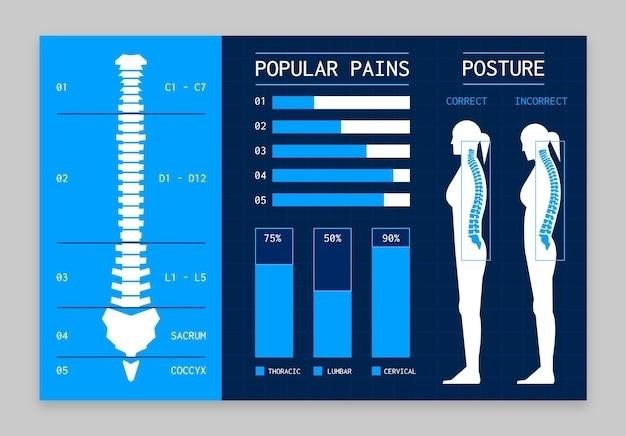
Maintaining the integrity of the surgical incision is paramount during the initial postoperative phase. Meticulous wound care, following the surgeon’s specific instructions, is essential. This typically includes regular dressing changes and monitoring for signs of infection such as redness, swelling, increased pain, or drainage. Patients are instructed on proper hygiene practices to minimize the risk of contamination. The use of a surgical brace or corset, as prescribed, provides additional support and protection to the surgical site, limiting movement and preventing excessive strain on the healing tissues. Avoiding activities that could stress the incision, such as heavy lifting or strenuous physical activity, is critical. Patients are educated on proper posture and body mechanics to minimize stress on the lumbar spine. Regular follow-up appointments with the surgical team allow for ongoing monitoring of wound healing and prompt management of any potential complications. Early recognition and treatment of any wound-related issues are essential to ensure optimal healing and prevent delays in the rehabilitation process.
Pain Control and Mobility Progression
Effective pain management is crucial for successful rehabilitation after lumbar fusion. A multimodal approach, often involving medication, physical therapy modalities (such as ice, heat, or electrical stimulation), and patient education, is generally employed. The initial focus is on managing acute postoperative pain to allow for comfort and participation in early mobility exercises. Gentle range-of-motion exercises, within the limits prescribed by the surgeon and physical therapist, are introduced to prevent stiffness and promote healing. Progressive mobilization, starting with simple movements in bed and gradually progressing to sitting, standing, and ambulation, is a key component. Pain levels are carefully monitored, and the intensity and duration of activities are adjusted as needed to avoid exacerbating discomfort. The use of assistive devices, like walkers or canes, may be necessary to aid in mobility, particularly in the early stages. Regular communication between the patient, surgeon, and physical therapist facilitates adjustments to the pain management and mobility plan based on individual progress and tolerance. A gradual increase in activity is essential to prevent re-injury and promote functional recovery.
Phase 2⁚ Early Rehabilitation (4-8 Weeks)
This phase focuses on building upon the progress made in the initial postoperative period. The emphasis shifts from pain management and basic mobility to increasing activity tolerance and functional improvements. Patients typically begin more active range-of-motion exercises, progressing to strengthening exercises targeting core muscles, back extensors, and hip and leg muscles. The goal is to improve stability, endurance, and overall functional capacity. Activities of daily living (ADLs) are gradually incorporated into the rehabilitation program, such as walking longer distances, climbing stairs, and performing household chores within prescribed limits. Regular physical therapy sessions are vital during this phase, providing guidance, monitoring progress, and modifying the exercise program as needed. The physical therapist will closely monitor the patient’s response to each exercise, ensuring proper technique and preventing overexertion. Patients are educated on appropriate body mechanics for lifting, bending, and twisting to protect the surgical site and promote long-term stability. Progress is carefully monitored, and the intensity and duration of activities are gradually increased as tolerated. The objective is to prepare the patient for a safe and successful transition to the advanced rehabilitation phase.
Increased Activity Tolerance and Functional Improvements
During this phase of rehabilitation, the primary focus is on enhancing the patient’s ability to participate in daily activities without experiencing excessive pain or fatigue. This involves a gradual increase in the duration and intensity of physical activities. Patients will progress from short walks to longer distances, incorporating inclines and varied terrains as tolerated. Functional exercises simulate everyday movements, such as lifting light objects, bending, twisting, and reaching. These activities are performed under the guidance of a physical therapist to ensure proper technique and prevent strain on the spine. The therapist will monitor for any signs of increased pain or discomfort, adjusting the program accordingly. In addition to physical exercises, patients may participate in occupational therapy to improve their ability to perform tasks at work or home. This may include adaptive techniques for lifting and carrying objects, as well as strategies for modifying the work environment to reduce strain on the back. The overall goal is to achieve a level of activity tolerance that allows patients to resume their normal routines and activities of daily living with minimal limitations. Regular check-ups with the surgeon and physical therapist are essential to monitor progress and make necessary adjustments to the rehabilitation plan.
Strengthening and Endurance Building
This phase focuses on building strength and endurance in the core and lower extremity muscles. Exercises are carefully selected to target specific muscle groups while maintaining spinal stability. Initially, low-impact exercises like isometric contractions and gentle range-of-motion movements are emphasized. As strength improves, resistance training is gradually introduced using resistance bands, weights, or bodyweight exercises. The exercises focus on strengthening the abdominal, back, and hip muscles, which are crucial for spinal support and stability. Endurance training, such as walking, cycling, or swimming, is incorporated to improve cardiovascular fitness and reduce fatigue. The intensity and duration of these exercises are progressively increased as tolerated, while maintaining a neutral spine posture to protect the surgical site. Proper form and technique are critical to prevent re-injury. Regular monitoring of heart rate and perceived exertion levels ensures that the patient is challenged appropriately without overexertion. The therapist provides feedback and guidance to optimize exercise performance and prevent compensatory movements that could strain the spine. This phase progresses towards more challenging exercises to prepare patients for a return to more strenuous activities.
Phase 3⁚ Advanced Rehabilitation (8-12 Weeks)
This phase focuses on a return to more demanding activities and increased exercise intensity. Patients progress from basic exercises to more complex movements that simulate real-life activities. The goal is to improve functional capacity and prepare for a return to work or recreational activities. Advanced exercises such as plyometrics (jump training), agility drills, and sport-specific exercises may be incorporated, depending on the individual’s goals and tolerance. Emphasis is placed on proper body mechanics and posture education to prevent future back problems. The therapist provides guidance on lifting techniques, proper posture while sitting and standing, and ergonomic adjustments in the workplace or home environment. Patients are educated on how to identify and avoid activities that could exacerbate back pain. This phase involves a gradual increase in the duration and intensity of activities, and regular monitoring for pain or discomfort is crucial. The program includes a detailed plan to progressively increase the load and difficulty of exercises, while ensuring the patient’s safety and comfort. The ultimate goal is a safe and successful return to a normal level of activity.
Return to Functional Activities and Increased Intensity
Posture Education and Body Mechanics
This phase emphasizes correcting posture and improving body mechanics to prevent future back problems and promote long-term spinal health. Patients receive comprehensive education on proper posture while sitting, standing, and lifting objects. This involves learning techniques to maintain a neutral spine alignment, minimizing strain on the fused segments. The focus is on strengthening core muscles to provide support and stability to the spine, reducing the reliance on compensatory movements. Instruction on safe lifting techniques is crucial, ensuring patients understand how to lift and carry objects without putting undue stress on their backs. Ergonomic assessments of the patient’s workspace and home environment are conducted to identify and rectify potential risk factors contributing to poor posture. Patients are taught how to adjust their workstation to promote proper posture and minimize strain. Regular practice of these techniques is encouraged, and patients are given exercises to reinforce proper body mechanics throughout their daily routines. This phase ensures long-term success and minimizes the risk of recurrence.
Phase 4⁚ Long-Term Management (12+ Weeks)
This phase focuses on maintaining the gains achieved during previous rehabilitation stages and preventing future back problems. It emphasizes the importance of continued exercise and activity modification to support spinal health. Patients learn a personalized exercise program focusing on core strengthening, flexibility, and endurance. This program is designed to be integrated into their daily lives, ensuring long-term adherence. Regular follow-up appointments are scheduled to monitor progress and make adjustments to the exercise program as needed. Education on proper body mechanics and posture continues to reinforce the techniques learned during earlier phases. Emphasis is placed on avoiding activities that could potentially strain the spine and understanding the importance of maintaining a healthy weight. Patients are encouraged to participate in low-impact activities that promote cardiovascular health and overall well-being while protecting their spine. The goal is to empower patients with the knowledge and tools to manage their spinal health independently and prevent future complications. This phase ensures a smooth transition back to their normal activities and long-term maintenance of their spinal health.
Maintenance and Prevention of Recurrence
Long-term success after lumbar fusion hinges on consistent adherence to a structured maintenance program. This involves a personalized exercise regimen emphasizing core strengthening, flexibility, and low-impact cardiovascular activities. Regular participation in these exercises helps maintain spinal stability and reduces the risk of future problems. Proper posture and body mechanics are crucial; patients continue to receive reinforcement on techniques to minimize strain on the spine during daily activities. Maintaining a healthy weight is vital as excess weight places additional stress on the spine. A balanced diet and regular physical activity contribute to weight management and overall well-being. Patients are taught to recognize and avoid activities that could exacerbate back pain or potentially lead to recurrence. This includes understanding their individual limitations and modifying activities accordingly. Regular check-up appointments with healthcare providers are essential for monitoring progress, addressing any concerns, and making necessary adjustments to the maintenance program. Open communication with the healthcare team ensures proactive management and prevents potential complications. The ultimate goal is to empower patients to take an active role in managing their spinal health and living a full and active life.